https://www.mirecc.va.gov/docs/visn6/2_Primary_Care_PTSD_Screen.pdf
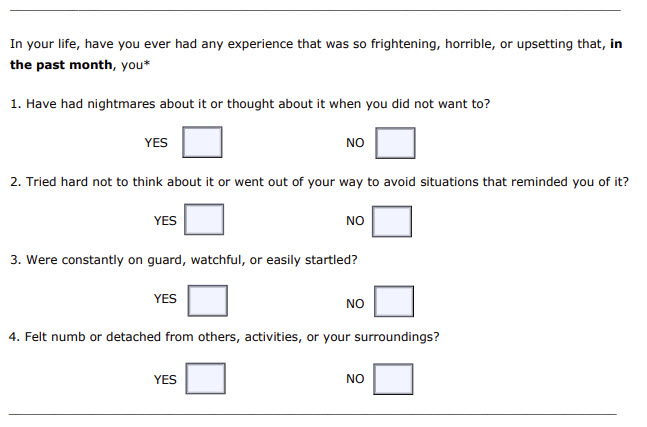
Current research suggests that the results of the PC-PTSD should be considered “positive” if a patient answers “yes” to any three items.
A positive response to the screen does not necessarily indicate that a patient has Posttraumatic Stress Disorder. However, a positive response does indicate that a patient may have PTSD or trauma-related problems and further investigation of trauma symptoms by a mental-health professional may be warranted.
If the PC-PTSD screening instrument is utilized, clarify responses to determine:
a. Whether the patient has had a traumatic experience
“I notice from your answers to our questionnaire that you experience some symptoms of stress. At some point in their lives, many people have experienced extremely distressing events such as combat, physical or sexual assault, or a bad accident, and sometimes those events lead to the kinds of symptoms you have. Have you ever had any experiences like that?”
b. Whether endorsed screen items are really trauma-related symptoms
“I see that you have said you have nightmares about or have thought about an upsetting experience when you did not want to. Can you give me an example of a nightmare or thinking about an upsetting experience when you didn’t want to?”
If a patient gives an example of a symptom that does not appear to be in response to a traumatic event (e.g., a response to a divorce rather than to a traumatic event), it may be that he or she is ruminating about a negative life event rather experiencing intrusive thoughts about a traumatic stressor.
Whether endorsed screen items are disruptive to the patient’s life
“How have these thoughts, memories, or feelings affected your life? Have they interfered with your relationships? Your work? How about with recreation or your enjoyment of activities?”
Positive responses to these questions in addition to endorsement of trauma symptom items on the PCPTSD Screen indicate an increased likelihood that the patient has PTSD and needs further evaluation.
Discern whether traumatic events are ongoing in a patient’s life
If ongoing traumatic events are a part of the patient’s life, it is critical that the primary care practitioner discern whether the patient needs an immediate referral for social work or mental-health services. The practitioner might ask:
“Are any of these dangerous or life-threatening experiences still continuing in your life now?”
If ongoing family violence is suspected, it is imperative that the patient be told the limits of confidentiality for medical professionals, who are mandated to report suspected ongoing abuse of children and dependent adults. Discussion of possible abuse should take place in the absence of the suspected perpetrator; if the abuser is present, victims may deny abuse for fear of retaliation.
If ongoing threats to safety are present:
- Acknowledge the difficulty in seeking help when the trauma has not stopped.
- Determine if reporting is legally mandated. If it is, develop a plan with the patient to file the report in a way that increases rather than decreases the safety of the patient and his or her loved ones.
If reporting is not appropriate, provide written information (or oral if written might stimulate violent behavior in the perpetrator) about local resources that might help the situation. Establish a plan that the patient will agree to in order to move toward increased safety. The National Domestic Violence Hotline is available to guide callers to local resources: 1-800-799-SAFE or TTY: 1-800-787-3224.